Rush Leads in Fight Against Substance Misuse
Tuesday, July 16, 2019

The National Institute on Drug Abuse recently awarded Rush University System for Health a $2 million grant to establish the Great Lakes Node of the NIDA Clinical Trials Network. The node is one of 18 research centers established nationwide to improve the delivery of scientifically based treatments to substance misuse patients, and to link treatment providers and patients across country.
Under the leadership of co-principal investigators Niranjan S. Karnik, MD, PhD, The Cynthia Oudejans Harris, MD, Professor of Psychiatry, and Mark H. Pollack, MD, the chairperson of the Rush Department of Psychiatry, the Great Lakes Node will develop and test interventions for substance misuse through the implementation of cutting-edge clinical trials. Through partnerships with experienced investigators representing major academic medical centers in the greater Chicago and Wisconsin areas, the node will serve as a vital Midwestern hub for the Clinical Trials Network.
Rush will serve as the lead institution that brings together the University of Illinois at Chicago, University of Chicago, Loyola University Medical Center, Lurie Children’s Hospital of Chicago, Northwestern Memorial Hospital, and UW Health and Medical College of Wisconsin as members of this group.
Tackling Substance Use Disorders
Friday, January 4, 2019

According to the National Institute of Drug Abuse, substance use disorders cost the U.S. more than $740 billion annually due to the crime, lost work productivity and health care expenses associated with addiction. At Rush, clinicians, researchers and faculty tackle the problem of addiction from multiple angles, embracing a practical, nonstigmatizing, person-based approach to prevention, screening and intervention.
Exploring alternatives to opioids
As a researcher, clinical psychologist John Burns, PhD, focuses on the management of chronic pain, a condition that often leads to opioid misuse and abuse. “My work focuses on changing how people look at their pain and how they can make changes in their behavior to alleviate their pain,” Burns says. “Physical therapy, exercise, cognitive behavioral therapy, yoga, Tai Chi — these are all preferred ways to manage chronic pain as opposed to opioids.”
But these approaches — especially CBT, which the CDC recommends as the first line of treatment — aren’t always accessible. That’s why Burns also considers other approaches, such as mindfulness, as additional pain management tools. In addition, he is researching the protective nature of endogenous opioid function, or what’s known as runner’s high, in reducing chronic pain. Ultimately, he hopes to give health care providers evidence-based alternatives to prescribing opioids.
Training physicians
Addiction medicine specialist Gail Basch, MD, is taking the lessons learned from her years of caring for patients with addiction disorders in the clinical setting and using them to train medical students, residents and fellows. She has seen tremendous change since her own training.
“When I did my residency more than 30 years ago, we rarely diagnosed or treated substance use disorders,” she says. “Today, our students and residents do that and more, including prescribing the latest FDA-approved medications for alcohol, tobacco and opioid use disorders. They learn to avoid stigmatizing terms, recognize the importance of provider and patient teamwork, and use a disease model. We understand now that absolute abstinence is not always the endgame — patients do best with a menu of choices.”
Lack of options drives health care providers to prescribe opioids
Friday, June 30, 2017
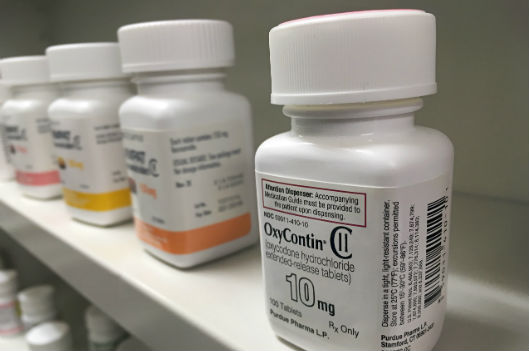
Opioid overdoses claim 91 lives a day, and nearly two-thirds of these deaths are attributable to prescription pain killers.
At times blame for this tragedy has fallen on the health care providers who write opioid prescriptions. But in a recent opinion piece for The Hill, two Rush University College of Nursing faculty members believe this blame is sometimes misplaced.
Melissa Kalensky, DNP, FNP, assistant professor, and Mona Shattell, PhD, RN, FAAN, professor and chair of the Department of Community, Systems and Mental Health Nursing, detail how lists of drugs covered by private insurance companies and public entities such as Medicaid and Medicare dictate what providers can and can’t prescribe to patients for pain management.
These lists contain limited non-narcotic options. Likewise, effective non-medication options are often cost prohibitive, with little or no coverage by insurance. And while there are genuine instances of those overprescribing or fraudulently prescribing opioids, in other cases well-meaning providers, who are ethically obligated to treat pain, can only prescribe what a patient can afford.
But at least one large entity, the Department of Veterans Affairs, is exploring alternatives to medication to help treat its service member patient base, many of whom are returning from active duty with chronic pain and other ailments.
